The Missing Piece in Cancer Recovery: Why Medical Nutrition Therapy Deserves a Permanent Place in Cancer Care
Exercise alone cannot fully carry the physiologic burden of cancer therapy. Quality nutrition, restorative sleep, and effective stress reduction all work in concert to influence how the body tolerates treatment and how well it recovers.
12/9/20252 min read
My post content
Strong After Cancer has always highlighted the power of movement, whether it be strength or aerobic training across the cancer continuum. Exercise play a crucial role in helping patients maintain function, support treatment tolerance, and restore a sense of agency during recovery. But movement alone is not enough. Quality nutrition, restorative sleep, and effective stress reduction collectively shape how the body withstands treatment and how successfully it rebounds afterward.
A new narrative review in Current Nutrition Reports underscores this reality: medical nutrition therapy (MNT) is not supportive care, it is evidence-based cancer treatment.
Malnutrition affects between 30 and 90 percent of people undergoing cancer therapy, yet more than 66 percent never receive adequate nutrition support. This gap contributes to higher toxicity, reduced treatment tolerance, longer hospitalizations, and worse overall outcomes. The review makes clear that malnutrition is not an inevitable side effect; it is a modifiable clinical condition that directly influences survivorship.
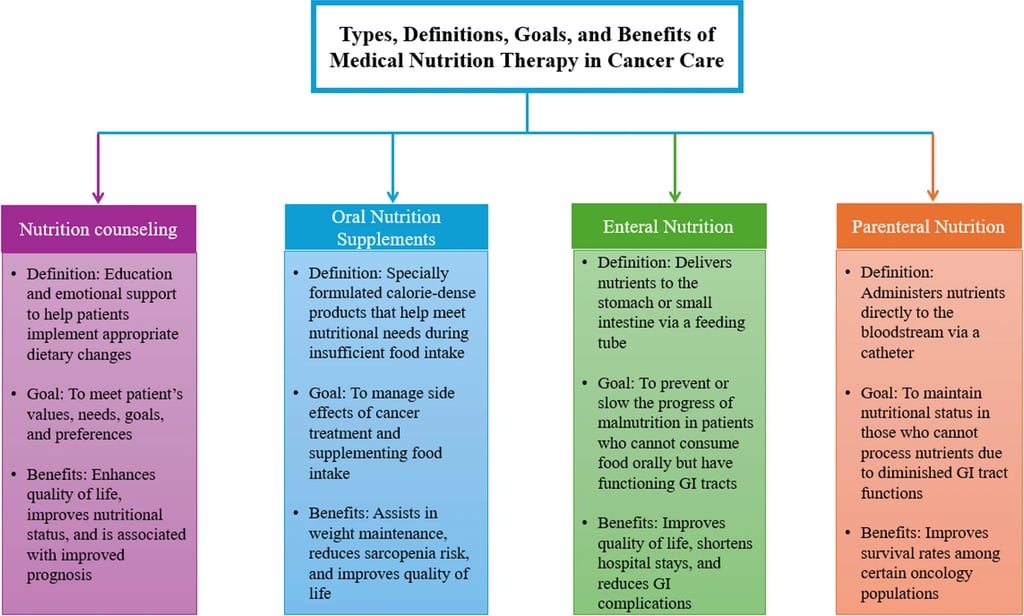
MNT includes individualized nutrition counseling, oral nutrition supplements, and, when needed, enteral or parenteral nutrition. Across multiple cancer populations, these interventions consistently maintain body weight and muscle, improve energy intake, reduce gastrointestinal and treatment-related symptoms, shorten hospital stays, and enhance quality of life. Nutrition support functions as treatment, not an optional extra.
Yet access remains limited. The average outpatient cancer center has one dietitian per 2,308 patients, far from the recommended ratio of 1:120. Only 53 percent of centers screen for malnutrition, and Medicare does not cover MNT for cancer diagnoses. These structural gaps disproportionately affect rural communities, low-income patients, and many Black and Hispanic populations, contributing to avoidable disparities in treatment experience and survivorship.
The science is clear that recovery is strongest when multiple lifestyle pillars work together. Exercise supports metabolic health, physical function, and treatment tolerance. Sleep restores immune balance and cellular repair. Stress reduction lowers inflammation and strengthens emotional resilience. Nutrition is the foundation that fuels all of these processes, providing the physiological support needed for patients to move, heal, and rebuild.
The review outlines a needed roadmap: expanding Medicare coverage for MNT, hiring more oncology dietitians, integrating nutrition education into medical training, improving screening and referral processes, and partnering with community-based Food-is-Medicine programs. These steps are essential for creating a cancer care system that supports not just treatment completion but true recovery.
Strong After Cancer sits at the intersection of science, movement, nourishment, and survivorship. The evidence continues to affirm one guiding principle: patients do better when exercise, nutrition, sleep, and stress management are integrated and not treated as separate or optional components of care. By aligning practice with the science, we can help more survivors safely return to running, cycling, lifting, and living fully after cancer.
Based on Gloss & Bhurosy (2025), Current Nutrition Reports.
